Reviewed by Sahil Chopra, MD, and Stacey Gunn, MD.
Apple's Continuing Effort in Advancing the Health Space
Every year, Apple hosts their annual conference in which they announce their latest innovations. This year, the AirPod Pro just got a huge upgrade. Starting with the new AirPod Pro 3, these wireless earbuds will begin to monitor heart rate and track a person’s workout. Apple boasts that these earbuds can detect over 50 different types of workouts, marking a turn in how they go about their fitness sector. To do this, the new AirPods will come equipped with a custom photoplethysmography (PPG), a small optical device that uses infrared absorption and reflection of light to detect changes in blood volume, similar to the SleepImage device that we at Empower Sleep use. Apple’s device shines this infrared light 256 times per second and combines the absorption data with the other sensors (such as the accelerometer, gyroscope, and their new AI model) to track a person’s heart rate and overall workout progress.
All of these new features mark Apple’s continuing effort to provide high quality health data at a consumer level. While Apple is in no way a replacement for a doctor, the data and insights provided by the devices can be used by medical professionals to better help diagnose and treat any conditions a person may have. Last year, Apple released sleep apnea detection on their Apple Watch (which we will discuss more below). At Empower Sleep, we allow for the integration of this data to better help us gain insights on our patient’s sleep so that we can better assess how we can help them. However, this is not to say that we only use Apple Watch data. Instead, we combine this with our own sleep testing data so that we can have better insights into our patients' sleep.
Sleep Apnea Detection on Apple’s Watch: A New Frontier in Health
Although general sleep tracking has been available for years on many wearable devices, in September 2024 the Federal Drug Administration (FDA) granted approval for the use of an Apple Watch to identify sleep apnea. Apple has successfully tied certain movements detected during sleep to those involved in sleep apnea. Thousands of peoples’ clinical sleep data were used to tie movements distinguished by an Apple watch to breathing disruptions. The technology is compatible with Apple Watch Series 9, 10, and Ultra 2.
What is Sleep Apnea?
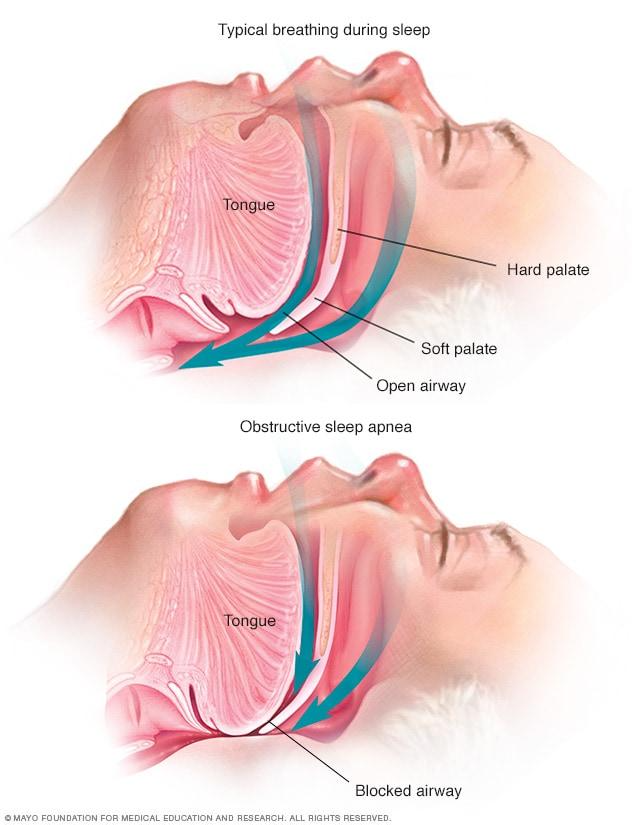
Many people with sleep apnea are undiagnosed and untreated. Sleep apnea occurs when the muscles that keep your tongue from blocking your airway relax while you sleep. This can cause sleep interruptions 5-60+ times in an hour as you wake up to breathe (see Figure 1). Bed partners may notice snoring, gasping, choking, or breathing cessation. Many people also have insomnia or excessive daytime sleepiness, but some patients are asymptomatic.
Why is Apple’s Sleep Apnea Detection Important?
Before home sleep testing was developed, sleep apnea could only be diagnosed through a single night’s sleep test in a clinical laboratory. This method, where a patient sleeps one night in a different environment from their home, certainly has clinical advantages in the amount of comprehensive data that can be collected, but has the potential to misdiagnose people by only have a snapshot of a single night, rather than the benefit of how the patient does over time. For example, if a person goes for a sleep study on a night that they have cold symptoms, then it is possible for sleep apnea to be overestimated. Or if their body position (side vs back) is different in the sleep lab than it typically is at home, then then results might not be reflective of real life for them.
Unlike a single snapshot of data from a clinic, Apple collects data over a month to ensure a pattern of sleep disturbances before alerting the watch wearer of possible sleep apnea. Aggregating data over a month allows a sort of “movie” to evolve of a patient’s sleep data instead of using a single frame in time. Once alerted, a person can download a PDF containing a month of their sleep data to take to a health provider, such as Empower Sleep, for review, which would prompt a formal sleep test for diagnosis and treatment.
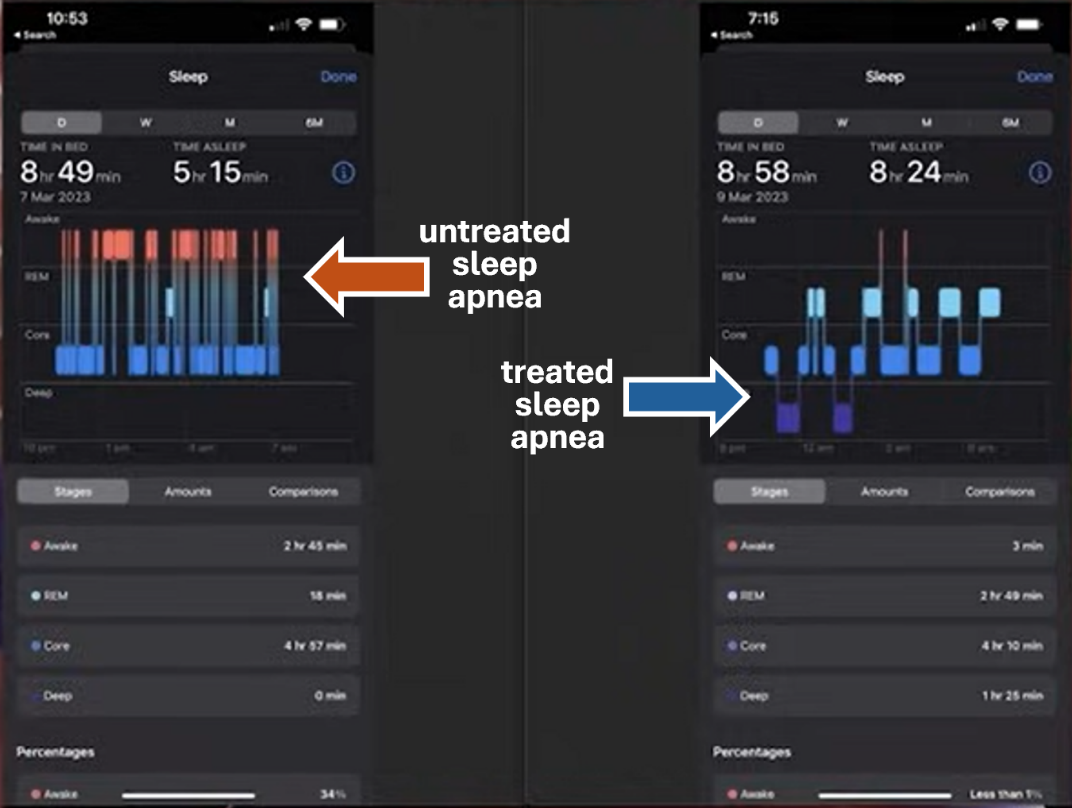
Figure 2 shows a single person’s sleep data from two nights on Apple’s sleep tracking. The left side shows a typical night’s sleep for this person before being treated with a continuous positive air pressure (CPAP) machine, and the right side shows the sleep data from the first night of treatment with a CPAP machine. Note the many orange marks indicating that the wearer is awake. The sleep disruptions caused by sleep apnea briefly jar the sleeper awake many more times on the left compared to the right. Their time asleep improved by almost three hours post-treatment with a CPAP machine. Their quality of life via increased daytime alertness significantly improved their day-to-day experiences.
Sleep disorders have a huge impact on the wellbeing of the world. Wearable health data, validated via the FDA, will help reduce undiagnosed sleep ailments and lead to a better quality of life for everyone. Sleep disorders are responsible for an estimated $130 billion dollars in damages for many of the following societal maladies:
- Car crashes
- Work related injuries
- Lost productivity
- Loss of life quality
- Premature death
It has been calculated that in the United States, roughly 810,000 collisions including 1400 fatalities are caused by sleep-deprived drivers. Most of these people do not even realize that they have a sleep disorder, they just know that they are tired all the time. Apple’s ability to collect and collate sleep data can help empower the wearer to seek out treatment.
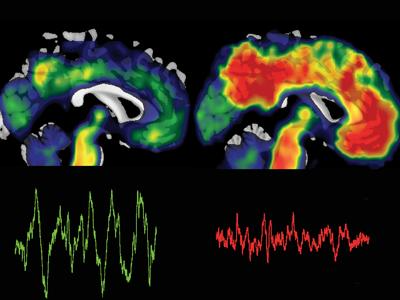
Sleep is one of the first cycles to break down when someone is ill. The ability to monitor sleep for years will give the wearer a baseline, which may be able to be used to help track changes over time and hopefully to see early patterns. Sleep disturbances can precede and predict the development of Alzheimer's disease, dementia, and Parkinson’s disease, and poor sleep is considered to be a modifiable risk factor.
What About False Alerts? When Should I See A Doctor?
The Apple Watch detection algorithm was specifically designed to help prevent people from unnecessarily wanting to see a doctor. The algorithm only monitors sleep if the feature is turned on and first looks at 30 nights worth of data. The data is scored using the AHI 4% scoring criteria (which is more specific than the more sensitive AHI 3% criteria) and only sends out an alert if there is consistent modterate-to-severe sleep apnea. This way, even if there are nights where a patient has a cold that makes it look like a person has sleep apnea, the device would not send out a false alert.
However, the AHI 4% rule can often rob people of treatment. Even if the Apple Watch doesn’t detect sleep apnea, that doesn’t mean that they may not have it. Instead, it could mean that they never turned the feature on, or that they have mild sleep apnea that isn’t being detected. Moreso, a person’s sleep can vary night-to-night, and inconsistent sleep apnea would not trigger an alert. Sleep apnea can also present in different forms, and if a person has a type of sleep apnea where their oxygen levels do not drop but their sleep is fragmented (this type is more common in women and those with a normal body-mass index), the Apple Watch algoritm will specfically not pick this type of sleep disordered breathing up.
Although the test as a 98.5% specificity (meaning the rate of false positives is very low), those who get an alert from their Apple Watch should get confirmatory testing to make an official diagnosis for insurance reasons. However, Apple did note in their study that those who did get a false-positive for moderate-to-severe sleep apnea did have mild sleep apnea. What this means is that those who get an alert should definitely act on it, but even those without an alert could still have sleep apnea. For more information on this, we encourage our readers to review Apple’s white paper (cited below).
In the years to come, we are looking forward to learning more and more about how longitudinal data can help us understand and modify our risks for chronic diseases!
References
Apple. “Introducing AirPods Pro 3, the Ultimate Audio Experience.” Apple Newsroom, 9 Sept. 2025, https://www.apple.com/newsroom/2025/09/introducing-airpods-pro-3-the-ultimate-audio-experience/.
Anwar, Y. (2015, June 1). Poor sleep linked to toxic buildup of Alzheimer’s protein, memory loss. Retrieved from https://news.berkeley.edu/: https://news.berkeley.edu/2015/06/01/alzheimers-protein-memory-loss/
Capoot, A. (2024, September 16). FDA clears Apple’s sleep apnea detection feature for use. Here’s how it works. Retrieved from CNBC.com: https://www.cnbc.com/2024/09/16/fda-clears-apples-sleep-apnea-detection-feature-for-use-heres-how-it-works.html
Dunn, N. (2024, September 12). New Apple Watch Series 10: Sleep Apnea Detection! Here's How It Works. Retrieved from https://www.youtube.com/@CPAPReviews: https://www.youtube.com/watch?v=YI-jq_RHpX8
Estimating Breathing Disturbances and Sleep Apnea Risk from Apple Watch . (2024, September). Retrieved from apple.com: https://www.apple.com/health/pdf/sleep-apnea/Sleep_Apnea_Notifications_on_Apple_Watch_September_2024.pdf
Faria, A., Allen, A. H., Fox, N., Ayas, N., & Laher, I. (2021, February 6). The public health burden of obstructive sleep apnea. Sleep Science, 14(3), 257-265.
Hanke, J. M., Schindler, K. A., & Seiler, A. (2022). On the relationships between epilepsy, sleep, and Alzheimer’s disease: A narrative review. Epilepsy & Behavior, 129, 108609.
Nanowear Announces FDA 510(k) Clearance for AI-enabled Continuous Blood Pressure Monitoring and Hypertension Diagnostic Management: SimpleSense-BP. (2024, January 4). Retrieved from Nanowearinc.com: https://www.nanowearinc.com/releasejan2024
Schrempf, W., Moritz , B. D., Storch, A., & Reichmann, H. (2014). Sleep Disorders in Parkinson’s Disease. Journal of Parkinson’s Disease, 4, 211-221.
Sleep Apnea. (2023, April 6). Retrieved from mayoclinic.org: https://www.mayoclinic.org/diseases-conditions/sleep-apnea/symptoms-causes/syc-20377631
Slowik, J. M., Sankari, A., & Collen, J. F. (2024). Obstructive Sleep Apnea. In StatPearls. Treasure Island, FL: StatPearls Publishing.
Winsky-Sommerer, R., de Oliveira, P., Loomis, S., Wafford, K., Dijk, D.-J., & Gilmour, G. (2019). Disturbances of sleep quality, timing and structure and their relationship with other neuropsychiatric symptoms in Alzheimer’s disease and schizophrenia: Insights from studies in patient populations and animal models. Neuroscience and Biobehavioral Reviews, 97, 112-137.


























































































%20thumbnail.jpg)
.png)