Reviewed by Sahil Chopra, MD, and Stacey Gunn, MD.
Research by Savit Malhotra.
Introduction
We have talked in much detail about how sleep apnea can harm the heart and the brain, but few realize that it may also silently steal your vision. In this article, we will focus on a disease known as glaucoma, a common but incurable eye disease that slowly damages your vision. Like the other diseases we have discussed, sleep apnea plays a role in the onset of this disease, and treating sleep apnea early on remains one of the key ways in which you can prevent major damage to your body. However, what makes this relationship different from most of the others is that this is a more unidirectional relationship. That is to say, sleep apnea can cause glaucoma, but the opposite is not true. In this article, we will break down the condition, the role that sleep apnea plays, and the importance of treating sleep apnea.
What is Glaucoma?
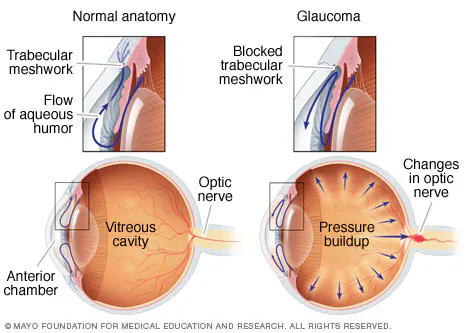
The human body consists of 12 key nerves (known as cranial nerves) that connect the brain to different parts of the body to aid in sensation and movement. One of these cranial nerves is known as the optic nerve (second cranial nerve), which is responsible for carrying visual information from the eyes to the brain.[1] Glaucoma is a condition where this nerve becomes damaged, impacting how visual information is sent to the brain (while there are three cranial nerves responsible for the eyes, the optic, oculomotor, and trochlear nerves, the latter two are responsible for eye movement, and glaucoma does not directly affect these nerves).[2] Typically, this damage to the optic nerve is the result of fluid buildup in the eye, leading to increased pressure on the optic nerve that damages it.[3] There are many different types of glaucoma, but for our purposes, we won’t spend too much time discussing these. For those who are interested, we encourage you to read more about glaucoma in reference 3.
In the United States, it is estimated that 1.62% of adults (roughly 4.22 million people) have glaucoma, with 0.57% (1.49 million people) having vision-affecting glaucoma.[4] Unfortunately, glaucoma can lead to permanent blindness/vision loss, especially when left untreated. Thankfully, treatment methods have evolved to allow people to delay, or even permanently prevent, the occurrence of total vision loss caused by glaucoma.[5] One way in which a person can help prevent themselves from developing vision loss is by treating the underlying causes of the glaucoma, one of which is sleep apnea.
How Do the Two Worsen Each Other?
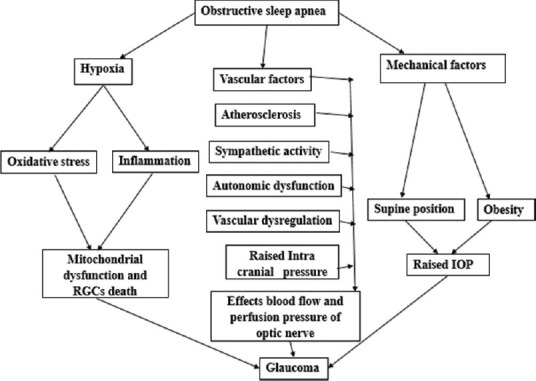
How sleep apnea causes glaucoma is still a topic that has some unanswered questions, like many of the other relationships we have discussed. What we do know with some degree of certainty is that those with sleep apnea are at a higher risk of developing glaucoma than those without sleep apnea.[6] Additionally, we do have a fairly good understanding of the pathophysiology behind the relationship, and it is similar to many of the other relationships that we have discussed. Like the other relationships, the key lies in oxidative stress caused by hypoxia. Hypoxia, which is where the body is oxygen-starved, leads to oxidative stress and inflammation in the body. In turn, retinal ganglion cells (a type of cell in the eye that helps with the transmission of visual information) develop mitochondrial dysfunction and become damaged or destroyed entirely, leading to glaucoma.[7,13] Another potential mechanism behind how sleep apnea can cause glaucoma relates to the vascular outcomes of sleep apnea. As we have talked about previously, sleep apnea leads to conditions such as coronary artery disease and heart disease (in addition to a number of other heart conditions). The American Academy of Ophthalmology has evaluated cardiovascular disease to be a significant risk factor for glaucoma.[8] This is another link that still remains unclear, but research has begun to establish a connection. One key theory is that those with heart disease also experience pressure changes in the blood vessels in the eyes, contributing to the buildup of pressure that damages the optic nerve. Another theory is that certain blood pressure medications can affect the flow of blood to the eye.[9] Regardless, it has been established that cardiovascular disease is a risk factor for glaucoma, and sleep apnea is a risk factor for cardiovascular disease. Thus, with untreated sleep apnea, glaucoma can potentially form as a result of the heart disease brought on by the sleep apnea.
What Happens When You Treat Sleep Apnea?
In a 2013 optometry meeting, it was stated and established that “sleep apnea may be a modifiable risk factor for glaucoma,” meaning that treating sleep apnea can also lead to better outcomes in lessening the chances of developing glaucoma.[10] This same conference advised that those with sleep apnea should also have a glaucoma screening due to the high correlation between the diseases. So, with sleep apnea increasing the risk of developing glaucoma, it makes sense to treat sleep apnea to mitigate the risk of glaucoma.[11] This is especially true if the severity of sleep apnea by itself warrants treatment.
But what about CPAP? Does CPAP help or harm glaucoma? A 2025 meta-analysis aimed to answer this question. This analysis looked at 15 studies with 495 total participants and concluded that there was, in fact, no statistically significant difference in intraocular (eye) pressure after CPAP. Interestingly, in some situations, researchers did notice a short-term rise in intraocular pressure during first time use of CPAP in a sleep lab. Other subgroups in the study did show a slight increase in eye pressure during long-term nightly CPAP use as well. Furthermore, the studies showed that CPAP was linked to a slight drop in blood flow to the eye. While slight blood flow drops aren’t usually too concerning, the eye, specifically the optic nerve, is very sensitive to oxygen and blood circulation, so even a minimal decrease can have an effect. However, there was no significant structural damage to the retina or optic nerve from the CPAP itself. Those who have glaucoma and are regularly using CPAP should also regularly have their eyes checked to ensure they are not experiencing any negative side effects from the therapy. While CPAP can cause some minor changes, regular monitoring can help keep any side effects in control, ensuring a balance between sleep and the health of a person’s eyes.[14]
What Should I Look Out For?
As we discussed in the previous article, the STOPBANG method remains an effective way for a person to help screen themself to see if they have sleep apnea. This test/acronym (posted below for reference) isn’t perfect, but it is still an incredibly useful tool.
- S - Snoring
- T - Tiredness during the day
- O - Obstruction (brief pause in breathing while sleeping)
- P - Pressure (high blood pressure)
- B - Body mass index of 30 or greater
- A - Age of 50+
- N - Neck circumference of greater than 16 inches (in women) or 17 inches (in men)
- G - Gender (male)
If you have three or more of the above-mentioned characteristics of sleep apnea, it is important that you see a sleep medicine doctor so that they can properly diagnose you and you can begin treatment. However, we will also mention that it is possible to have sleep apnea even with a low STOPBANG score, and so a normal score should not prevent someone from being evaluated if they are otherwise concerned.[12]
Unfortunately, due to there being many different forms of glaucoma, different symptoms can arise. In some cases, there may be no symptoms at all in the early stages, and over time, a person will begin to develop blind spots in their peripheral vision and eventually in their central vision (this is the case with open-angle glaucoma). In other types, such as acute angle-closure glaucoma, a person may experience headaches, eye pain, nausea or vomiting, blurred vision, colored rings around lights, and eye redness.[2] For more information, we encourage you to read reference 2 to go over the full list of symptoms for the different types of glaucoma. Glaucoma is a progressive disease, and so any changes in vision should be noted as soon as they arise. If there are drastic changes in your vision, you should see a medical provider (such as an ophthalmologist) as quickly as possible.
Conclusion
While there are still unknowns between the two diseases, there is still enough information to conclude that there is a clear relationship between sleep apnea and glaucoma. Those who are worried that they may have sleep apnea should see a sleep medicine specialist, and if they begin to notice changes in their vision, they should see an ophthalmologist quickly to lessen the impact of the disease. The effects of glaucoma can be permanent, especially when left untreated for a long time, and so being timely is important when it comes to this disease. The longer you wait, the worse the damage.





























































































%20thumbnail.jpg)
.png)