Reviewed by Sahil Chopra, MD, and Stacey Gunn, MD.
Research by Savit Malhotra.
Introduction
Last week, we began our discussion on how sleep apnea can contribute to diseases in the brain, looking specifically at dementia. In this article, we will continue our discussion by discussing how sleep apnea can lead to strokes or an increased risk of having a stroke. We have previously looked at the different heart diseases that can result from sleep apnea, and the mechanism behind how sleep apnea contributes to strokes is somewhat similar. Throughout this article, we hope to show that sleep apnea is not something that should be overlooked. By treating sleep apnea, one can greatly reduce their risk of developing some other disease that is far worse.
What is a Stroke?
A stroke, classified as either an ischemic stroke (reduced blood flow due to a blockage) or a hemorrhagic stroke (reduced blood flow due to bleeding), is a condition where the brain does not receive a normal amount of blood. During an ischemic stroke, the tissue of the brain is damaged due to a lack of oxygen and nutrients, leading to cell death. In a hemorrhagic stroke, a blood vessel ruptures, leading to bleeding in the brain. This increases the pressure in the head, causing the brain cells to be damaged.[1] In either case, the damage done to the brain is often permanent, and the longer a person waits before receiving treatment, the more damage there is. In a way, a stroke is similar to a heart attack. During a heart attack, the heart cells are damaged due to a blockage, similar to how brain cells are damaged during a stroke.[2]
Unfortunately, strokes are one of the leading causes of death globally, with the World Health Organization (WHO) placing it as the third leading cause in 2021, just below heart disease (first) and COVID-19 (second).[3] In 2022, 795,000 people had a stroke in the United States, with a new stroke case occurring roughly every 40 seconds.[4] Some researchers estimate that about 140,000 Americans die yearly because of a stroke.[5] Although strokes can be the result of a number of factors, such as genetics and past medical history, there are a number of ways in which a person can lessen their chance of developing a stroke. And one such way is by treating their underlying sleep apnea. However, a stroke can also lead to sleep apnea or the worsening of already existing apnea. There is more complexity to this since stroke damage can be irreversible. In the next few paragraphs, we will be breaking this all down.
How Do the Two Worsen Each Other?
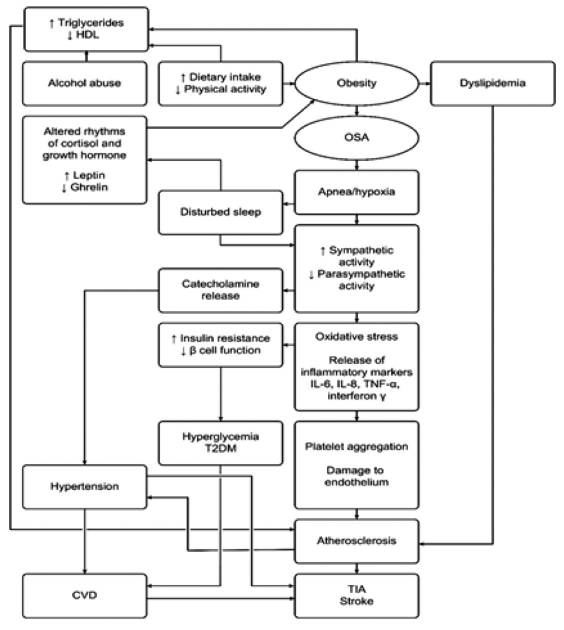
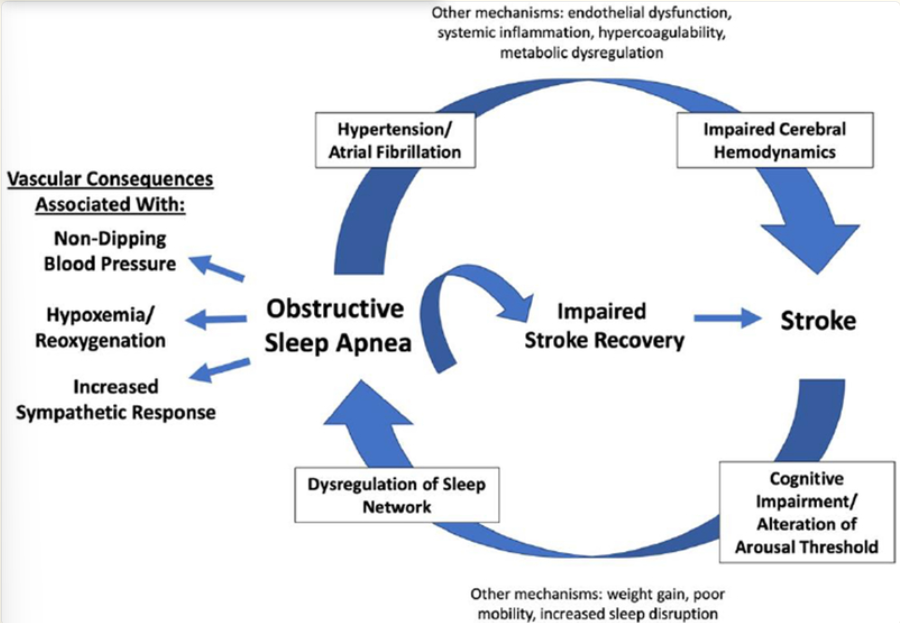
Sleep apnea, particularly obstructive sleep apnea, has been shown to be an independent risk factor for stroke, meaning that those with obstructive sleep apnea are more likely to have a stroke.[6] Research has pointed, once again, to the idea that oxidative stress is behind the increased risk. Those with obstructive sleep apnea experience increased inflammatory markers (the body’s way of indicating that there is inflammation in the body), which damage the inner walls of blood vessels. This damage leads to blood platelets clumping/clotting, which creates oxidative stress and further damage to the blood vessels. This damage is one pathway that can lead to stroke in patients with obstructive sleep apnea. Furthermore, obstructive sleep apnea can cause sympathetic nervous system activation, which, as we have discussed previously, is responsible for the “fight-or-flight” response in the body. This response causes the release of certain neurotransmitters, such as epinephrine and norepinephrine, which increase blood pressure. Increased blood pressure further worsens platelet clotting and damage to the blood vessels. In turn, there is an increased risk of stroke.[7] In this mechanism, we see that sleep apnea leads to two effects: oxidative stress and sympathetic nervous system activation. Independently, either effect can lead to stroke, but both can occur simultaneously, which only further increases the likelihood of stroke.
As we talked about in one of the previous articles, sleep apnea can also greatly increase your risk of atrial fibrillation.[16] When someone has atrial fibrillation, their heart beats at an irregular rhythm due to a mismatch between the upper and lower chambers. As a result, blood clots can form in the left atrial appendage. Once these clots are formed, it’s possible that they may be released from the heart and then travel to a person’s brain, leading to a stroke.[17] While this is not always the case, and atrial fibrillation does not always lead to blood clots, the longer that either condition (sleep apnea or atrial fibrillation) remains untreated, the more likely it is to lead to long term damage.
Sleep apnea, however, can also be the result of a stroke. A study published in the Stroke journal found that, after a stroke, the estimated occurrence of obstructive sleep apnea was between 43%-70% while the estimated occurrence in the general population was between 4%-24%.[8] Interestingly, this study found that obstructive sleep apnea after stroke was more common than central sleep apnea, with the occurrence of obstructive sleep apnea being between 30%-70% while the occurrence of central sleep apnea was between 6%-24%. Why this is the case is not entirely understood. Central sleep apnea occurs when the brain is unable to properly signal the body to breathe, whereas obstructive sleep apnea occurs when there is a blockage in the airway. If the brain is damaged due to a stroke, it would make sense that central sleep apnea is more likely to occur. After a stroke, the medulla can become weakened and less responsive to CO2 levels in the body, leading to central sleep apnea.[9] After a stroke, it is not uncommon for a person to experience dysphagia (difficulty swallowing), which can elevate airway resistance, leading to sleep-disordered breathing. Depending on the person and what specific areas of the brain are affected, the hypoglossal nerve (the cranial nerve responsible for swallowing) can also potentially become damaged, further contributing to an increased apnea-hypoxia index.[10] Combined, these mechanisms could help explain why obstructive sleep apnea is more common than central apnea following a stroke. Some part of the increased rates of obstructive sleep apnea may be that it is not recognized or treated, and instead only picked up after the stroke occurs. [8]
What Happens When You Treat Sleep Apnea?
As we have discussed, there is an increased likelihood of developing sleep apnea after a stroke. However, when left untreated, sleep apnea can greatly hinder a person’s recovery which is why many advocate for the early diagnosis and treatment of sleep apnea post-stroke.[11] For the treatment of sleep apnea, CPAP remains the gold standard and studies have found that it can even help with stroke-related symptoms. For example, studies found that, with patients who used CPAP, nonvascular outcomes (such as cognition and neurologic recovery) can be improved with post-stroke sleep apnea.[18] One meta-analysis explored this by looking at ten randomized controlled trials (with a total of 564 participants) and found that neurofunctional scales did show an overall improvement in neurological function, and one of the studies showed that CPAP improved long term survival.[19]
A topic that is still up for debate, however, is whether a CPAP machine can decrease the likelihood of a stroke. The issue here is that current studies have only looked at certain subgroups and on a more general level. For example, one study found that, in women, the elderly, and middle-aged men, there was an overall decrease in cardiovascular events as a whole, not specifically stroke likelihood.[12] So while the data suggests that a CPAP could help with decreasing overall cardiovascular events, there is limited data on strokes specifically, and even further limited data on the population as a whole. Another study found the risk of stroke was only decreased under certain conditions (when the severity of the obstructive sleep apnea was moderate-severe and the patients adhered well to their CPAP), but this too was only observed in cohort studies and the results were not consistent in randomized control studies.[21] In terms of stroke recurrence, a study on 101 patients there was a significant reduction of stroke recurrence and mortality when CPAP treatment was used.[20] Unfortunately, it is hard to reach a definitive conclusion, and performing a research study on this topic is difficult due to the ethical concerns of knowingly leaving someone with sleep apnea untreated.
What Should I Look Out For?
As we discussed in the previous article, the STOPBANG method remains an effective way for a person to help screen themself to see if they have sleep apnea. This test/acronym (posted below for reference) isn’t perfect, but it is still an incredibly useful tool.
- S - Snoring
- T - Tiredness during the day
- O - Obstruction (brief pause in breathing while sleeping)
- P - Pressure (high blood pressure)
- B - Body mass index of 30 or greater
- A - Age of 50+
- N - Neck circumference of greater than 16 inches (in women) or 17 inches (in men)
- G - Gender (male)
If you have three or more of the above-mentioned characteristics of sleep apnea, it is important that you see a sleep medicine doctor so that they can properly diagnose you and you can begin treatment. However, we will also mention that it is possible to have sleep apnea even with a low STOPBANG score, and so a normal score should not prevent someone from being evaluated if they are otherwise concerned.[13]
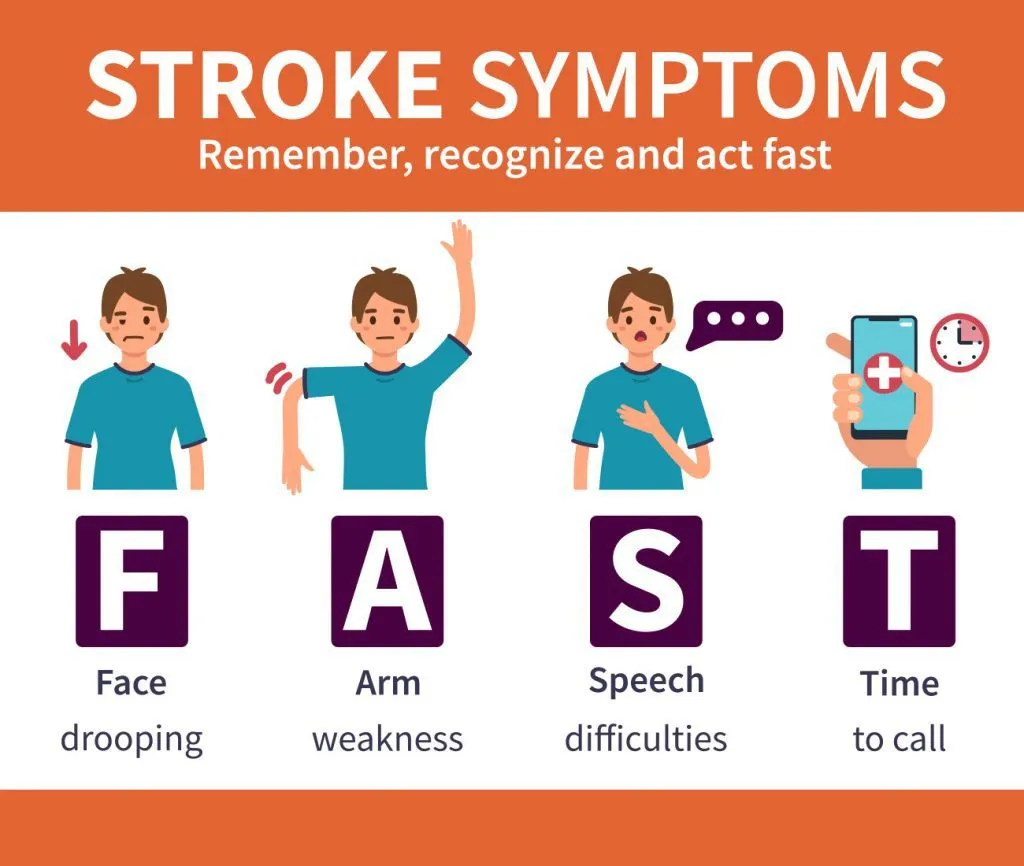
A stroke is a medical emergency and needs to be treated as quickly as possible. One common acronym used to help determine if someone is experiencing a stroke is FAST. F stands for face drooping, A for arm weakness, S for speech difficulties, and T for time to call.[14] If a person is experiencing these symptoms, it is important to call 911 immediately because the longer a person waits, the more their chances of survival decrease. Aside from these symptoms, a person experiencing a stroke may also present with numbness/weakness on one side of their body, confusion, impaired vision, difficulty walking, or a severe headache.[15]
Conclusion
A stroke is a medical emergency and needs to be treated as such. The long-term impacts of a stroke can be life-altering, and it is important to understand how you can decrease your risk of developing a stroke. One such way is by treating your sleep apnea. Although the data is unclear on the significance of treating sleep apnea when it comes to decreasing your risk of stroke, most of the time, sleep apnea warrants treatment regardless. A decreased likelihood of developing a stroke is a potential positive byproduct. What has been shown, however, is that the chance of developing sleep apnea post-stroke is significantly greater than in the general population. For this reason, it is important to be screened for sleep apnea if you have previously experienced a stroke. Doing so can help you recover better, mitigate your risk of further damage, and, in turn, live a healthier life.





























































































%20thumbnail.jpg)
.png)