Reviewed by Sahil Chopra, MD, and Stacey Gunn, MD.
Research by Savit Malhotra and Theresa Do.
Introduction
As we continue our discussion of the many ways that sleep and the skin are interconnected, we will spend this week touching on atopic dermatitis. Atopic dermatitis, better known as a type of eczema, is a condition that millions struggle with and one that has many ties to sleep. Eczema flare-ups can be triggered by the quality of your sleep, your sleeping environment, and a number of other sleep-related factors. For this reason, it is important to ensure that every aspect of your sleep regimen is top-tier. In this article, we’ll be breaking down what atopic dermatitis is, how it is related to sleep, and some things that you can do to ensure that your sleep isn’t getting in the way of the healthy skin you want.
What is Atopic Dermatitis
Atopic dermatitis is one specific type of eczema. Eczema is a chronic condition where the skin is unable to retain moisture and defend against environmental factors due to a damaged skin barrier.[1] Atopic dermatitis typically begins during infancy and causes dry skin, itchiness, bumps, rashes, and dark circles around the eyes.[2] While atopic dermatitis tends to go “dormant” after infancy (10%-30% of children are documented to have the condition versus 2%-10% of adults),[3] it is not uncommon for some people to experience flare-ups later in life.[4] Unfortunately, there is no cure for the condition, though treatments do exist to help manage flare-ups.
Three key components lead to atopic dermatitis: genetic predisposition, epidermal barrier disruption, and immune system dysregulation.[5]
- Like most aspects of our body, atopic dermatitis is heavily influenced by our genes. Twin studies have found that atopic dermatitis has an estimated heritability of ~75%, with the key mutation being in the gene that encodes filaggrin.[6] Filaggrin is responsible for building a strong skin barrier and producing natural moisturizing factors.[7] The loss of filaggrin thus leads to decreased skin moisture, characteristic of atopic dermatitis.
- Epidermal barrier disruption relates to the outermost layer of the skin, the stratum corneum, becoming damaged.[8] When this layer becomes damaged, the skin loses its moisture, and external irritants are more likely to affect the deeper layers of the skin, causing redness and dryness.[9] Those with atopic dermatitis experience this damaged barrier (likely partially due to the mutation of the filaggrin gene discussed earlier), hence the physical symptoms seen in those with the condition.
- Lastly, immune system dysregulation occurs when the immune system either overreacts, underreacts, or attacks the body’s own tissues mistakenly.[10] In those with atopic dermatitis, the body experiences an overreactive Type 2 immune response (the primary response that protects against parasites) due to the compromised skin barrier.[11,12] This overreactive response leads to chronic inflammation and itching.[13]

Sleep and Atopic Dermatitis
Sleep disturbances are a common symptom for patients with atopic dermatitis.[14,15] Similar to other dermatological conditions discussed in our blogs (see our articles on psoriasis and rosacea), sleep may have a bidirectional relationship with atopic dermatitis. In other words, sleep disturbances and low sleep quality can trigger atopic dermatitis flare-ups, and more severe atopic dermatitis can interrupt getting high-quality sleep. As you can imagine, it can be difficult to get a comfortable night’s rest when you are dealing with skin discomfort. Adult and children patients with atopic dermatitis report struggling with falling asleep, waking up in the middle of the night, and feeling tired or having excessive sleepiness during the daytime.[14] Specifically, in children, a literature review revealed that they are more likely to experience difficulties waking up in the morning as well as staying up longer after trying to sleep.[14] This may be due to the disease severity, symptoms, or potentially even underlying mechanisms associated with the disease.
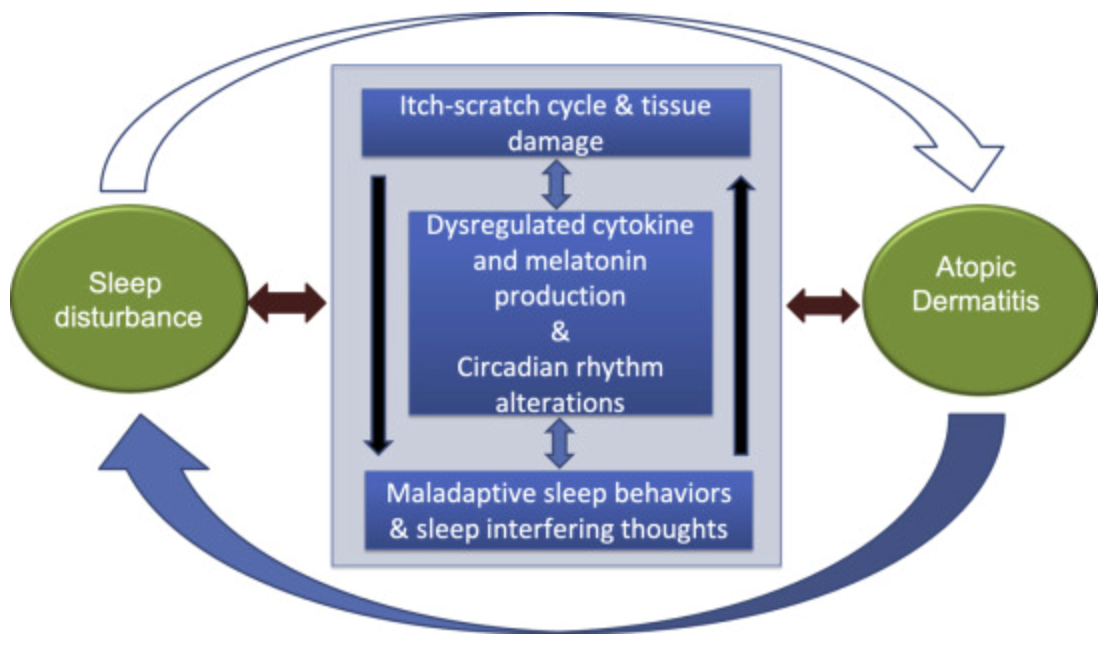
Researchers pose three potential mechanisms for how sleep and atopic dermatitis can relate to one another.[16] Firstly, stress of having atopic dermatitis can impact sleep quality by causing patients to have a higher risk of developing insomnia.[17] As patients deal with atopic dermatitis, they may grow fearful of having a flare-up during the night. This can further turn into rumination, which can prevent them from falling asleep. Secondly, the persistent itch or pruritus itself can cause sleep disruptions.[18] Beyond the psychological impacts of atopic dermatitis, sudden itch attacks make it extremely difficult to fall asleep and stay asleep. This scratching can also cause inflammation, which has been linked to further sleep disturbances.[19] Finally, researchers hypothesize that patients with atopic dermatitis have an altered expression of cytokines (messenger molecules in the immune system) that promote normal circadian rhythm and melatonin cycles, in particular cytokine IL-6.[16,[20] Additionally, melatonin patterns in many patients with atopic dermatitis seem to be disrupted.[21]
Conclusion
Atopic dermatitis is a condition that can affect not only what patients feel on the outside with their skin appearance, but also what they feel throughout the day. Managing the symptoms of atopic dermatitis to get better quality sleep involves a number of steps. The National Eczema Society recommends[22]:
- Sleep in a room with constant temperature. This can minimize the likelihood of flare ups from hot and stuffy environments.
- Maintain a clean environment. As atopic dermatitis can be triggered by environmental factors such as dust and dander, keeping a clean environment through routine sweeping and dusting can help reduce these triggers.
- Choose the right bedding. Feather bedding and memory foam can cause body heating and promote allergenic reactions. Opt for synthetic duvets and cotton materials.
- Have a good sleep routine. Try our healthy sleep tips in our recent article post.
If you are having trouble sleeping at night, don’t wait to make a change. Our care team at Empower Sleep can help you reach your sleep goals, while addressing other concerns you may have that can impact your beauty rest. Talk to a sleep coach today!


























































































%20thumbnail.jpg)
.png)